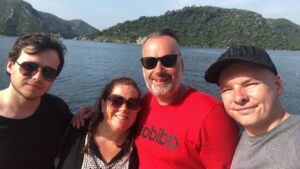
 Peter was our first born, big brother to Harry and loved deeply by many. He was someone who transcended individual friendship groups throughout school. Peter was so fondly thought of because of his kind nature that he fitted in everywhere.
Peter was our first born, big brother to Harry and loved deeply by many. He was someone who transcended individual friendship groups throughout school. Peter was so fondly thought of because of his kind nature that he fitted in everywhere.
He was caring, thoughtful, sensitive and funny, and he wanted to make life better for others whenever he could.
Peter was also a talented musician and music producer, and there wasn’t much he didn’t know about technology! He had a wonderful enquiring mind.
It is engraved on his headstone that he was too beautiful for this earth, and he truly was. We have always preferred to say, however, “Peter is”, not “was”. We believe fervently that Peter still exists but not in the way we long for.
Peter was 17 years old when he was diagnosed with front temporal lobe epilepsy and died when he was just 21. Aside from the limiting support we were able to give during those four years, he received minimal support elsewhere.
Stop the SUDEP silence
The first time we became aware of sudden unexpected death in epilepsy (SUDEP) was when we were informed of his cause of death. At no point while Peter was alive did any of the clinicians involved in Peter’s epilepsy care mention SUDEP or provide us with any SUDEP literature.
In a recent film I made with the aim to stop the SUDEP silence, I refer to and acknowledge a considered unconscious bias around this. Would I really have wanted to know about SUDEP when Peter was alive? The answer is unequivocally yes.
Of course, we would have been fearful and anxious as would have Peter, but, ultimately, we would have been empowered to help keep him safe. Any feelings of anxiety we may have felt at the time pale into insignificance compared to the trauma and finality of losing Peter forever.
If we had known about SUDEP from the start, we all would have understood the seriousness of his condition. We believe it would have made a significant impact on medication adherence, for one.
It would have also enabled us, as a family, to take safeguarding measures knowing about SUDEP and the risks associated with sleep seizures. We would have made adaptations to his sleeping arrangements and used a seizure detection device and an anti-suffocation pillow.
We would have also had a far better understanding of Peter’s vulnerability whilst being away from home at university.
I have epilepsy. Am I at risk of SUDEP?
Epilepsy Action’s information says:
SUDEP is rare, affecting around 1 in every 1,000 adults with epilepsy each year. This figure is for people with epilepsy in general. Your individual level of risk will depend on what type of seizures you have and how well-controlled they are. No one can say exactly who will be affected by SUDEP, but research has shown there are some things that can put you at a higher risk.
Risk factors of SUDEP
The risk factors for SUDEP include:
- Tonic-clonic seizures
- Sleep seizures
- Missing doses of seizure medicines
- Alcohol or drug dependency
- Living alone
What can I do to reduce the risk of SUDEP?
- Take your seizure medicines every day as prescribed – speak to your doctor if you have any concerns with your medicines, such as side effects.
- Try to avoid situations that could trigger your seizures, such as lack of sleep, drinking too much alcohol and stress.
- If your seizures are not fully controlled, ask to be referred to an epilepsy specialist for a review of your epilepsy.
- Keep a seizure diary to help you track what is happening.
- Think about sleeping and living arrangements – having someone there could help if you have a seizure. If you live alone, a safety check plan could help.
- Consider alarms and monitors, safety pillows and sleeping on your back.
‘You matter’
 What we would like to see happen in the future around SUDEP communication is for people living with epilepsy to be informed about SUDEP in clear terms. To have health professionals not avoid using the word SUDEP, and what that means, by only talking about generic ‘risk’.
What we would like to see happen in the future around SUDEP communication is for people living with epilepsy to be informed about SUDEP in clear terms. To have health professionals not avoid using the word SUDEP, and what that means, by only talking about generic ‘risk’.
We are often asked how clinicians should deliver the SUDEP conversation. First and foremost, SUDEP just simply needs to be spoken.
Similarly to discussions oncologists and cardiologists have with their patients, the informing of SUDEP will be extremely difficult and challenging, however this information must be given. There is no easy way, it is as simple as that. It just takes courage, kindness and time.

My personal opinion is that people living with epilepsy are among the most courageous. I can’t even begin to imagine how it must be to manage this complex neurological condition.
From personal experience being Peter’s mum, and in the work I have done these past five years running the epilepsy charity, the Peter Doody Foundation, I feel that people living with epilepsy are not getting the optimal care and support they should.
These past two years I have been making a film titled ‘Stop SUDEP Silence’ which was released on the 8th of July this year on what would have been Peter’s 27th birthday. The film includes accounts of parents who have lost a child to SUDEP, parents of children living with epilepsy, clinicians and someone living with epilepsy.
People don’t like talking about SUDEP. But we have to.
You matter, unbelievably so.
Such a ‘mum’ thing to say I know, but do take your medication as prescribed. Ask your clinicians about SUDEP and the risk factors. Ensure you are given information relating to seizure detection devices and safeguarding aids. Understanding fully about your diagnosis and SUDEP can be empowering. It will help keep you safe.
For more support and information please call our helpline on 0808 800 5050, visit Epilepsy Action or the Peter Doody Foundation.




